Blog | 11/13/2024
Chronic Care Management on the Rise: The Boom of CMS Codes and Companies in the Space
By Greg Chittim, Partner and Managing Director, Jeffrey Abraham, Partner and Shreya Saraf, Director
One of the lasting impacts of the Covid-19 pandemic is the sustained utilization and expansion digital health is rapidly transforming chronic care management, leveraging technology to enhance patient engagement, improve outcomes, and streamline healthcare delivery. This development is supported by CMS’ reimbursement codes, with new codes and rising uptake of existing ones.
RPM has gained significant traction due to expanded reimbursement policies from the Centers for Medicare & Medicaid Services (CMS), which have led to a dramatic increase in utilization. Since the introduction of RPM billing codes, Medicare payments surged from $5.5 million in 2019 to $101.4 million in 2021, reflecting the value and market capture of patient monitoring technologies.
In contrast, RTM is also on the rise but at a more measured pace, as CMS introduced five new codes in 2022 to enhance reimbursement for therapeutic monitoring services. These codes allow healthcare providers to bill for non-physiological data collection, thus opening new avenues for financial compensation.
RTM codes nicely complement RPM codes in the use of chronic disease management technologies – while RPM uptake has been concentrated in cardiology, nephrology and a few other specialties, RTM opens up access to digital physical therapy with physical medicine and rehab accounting for nearly half of all claims.
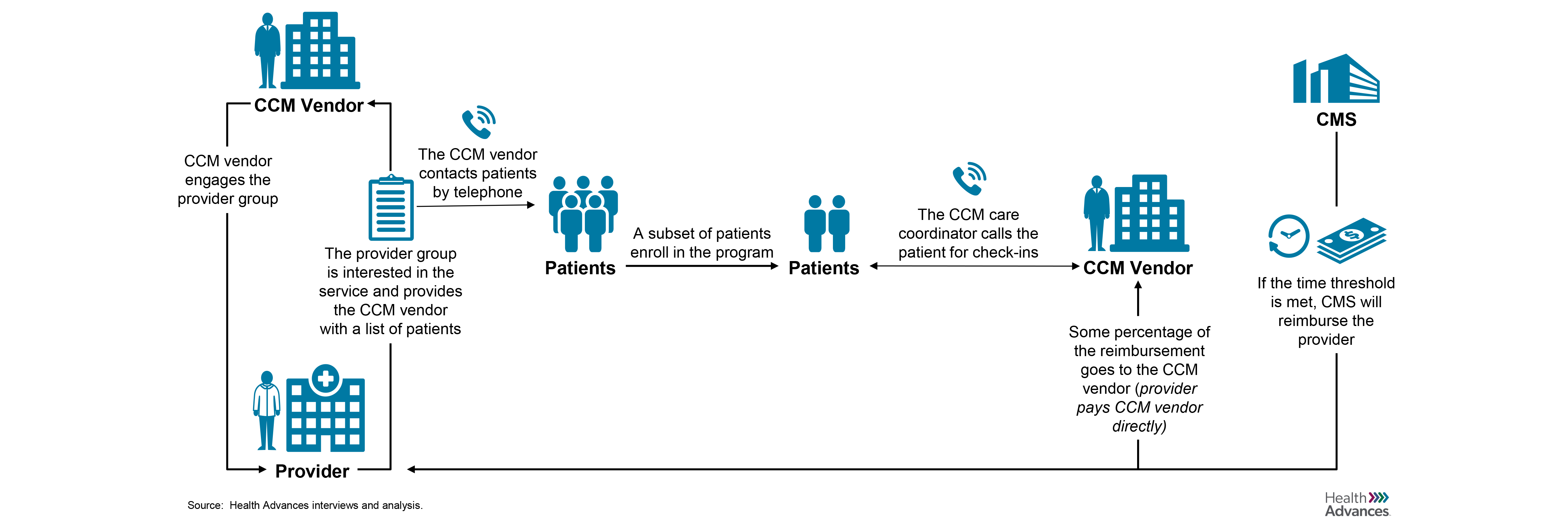
On the other hand, the uptake of Chronic Care Management (CCM, established in 2014) and Principal Care Management (PCM, introduced as a Part B benefit in 2022) codes has been disappointingly low despite potential benefits. This is not surprising though, given the limited awareness among providers, complexity of the coding system, and the requirement for coordination among multiple providers.
The multiple time-based codes for once-monthly services complicates billing processes, leading to confusion and hesitance among practices. Additionally, since only one provider can bill for CCM or PCM services per patient each month, careful coordination within the care team is required, complicating implementation further. Practice economics play a large role too as practices may struggle to absorb the startup costs associated with implementing these services and hiring staff for care coordination.
The newest kid on the block, APCM (Advanced Primary Care Management, introduced as part of the 2025 Medicare PFS) aims to streamline care management by integrating and simplifying elements from CCM and PCM. Unlike its predecessors, APCM eliminates time-based billing, reducing administrative burdens for healthcare providers. It introduces three new HCPCS codes (G0556, G0557, G0558) based on patient complexity and chronic conditions. However, challenges such as perceived insufficient reimbursement rates compared to other concurrent billing services may hinder adoption, especially among smaller practices. Additionally, the requirement for patient consent and the complexities of billing will continue to overwhelm providers, leading to reluctance in fully engaging with APCM codes.
As the healthcare landscape evolves toward value-based care, the integration of all these codes will be crucial in addressing the needs of patients with chronic diseases. Ultimately, these trends point toward a future where chronic care management is more efficient, accessible, and patient-centered, leading to improved health outcomes and reduced healthcare costs.
Authors
- Greg Chittim, Partner and Managing Director, Co-leads Health Advances’ Health IT and Digital Health practice
- Jeffrey Abraham, Partner, Co-leads Health Advances’ Health IT and Digital Health practice
- Shreya Saraf, Director, member of Health Advances’ Health IT and Digital Health practice

